Written by Kaya van der Horst
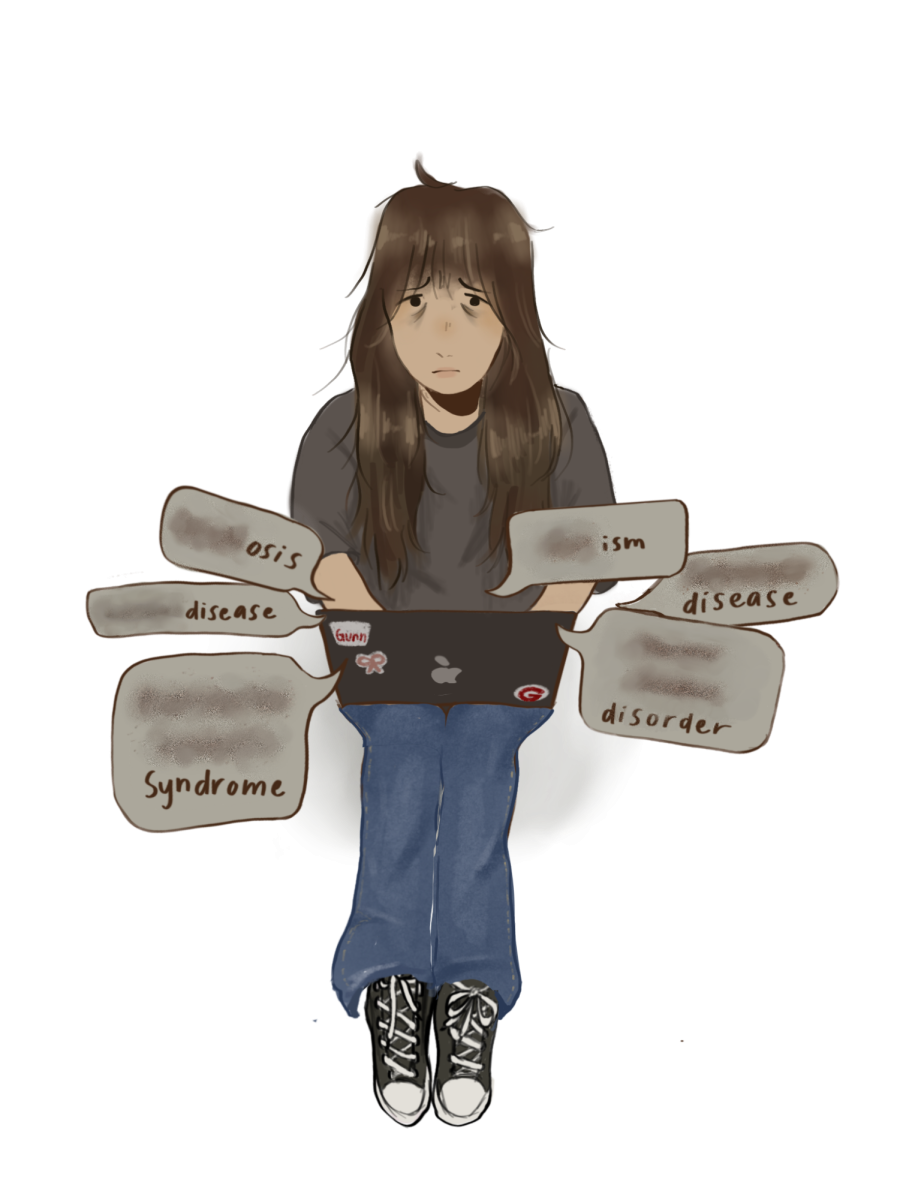
The Children’s Health Council (CHC) launched its first Intensive Outpatient Program (IOP) on May 8, marking a pivotal point in expanding local teen mental health services. The program will address the needs of high school teens ages 14 to 18 who show signs of significant anxiety, depression or suicidal thoughts.
According to CHC Head of Adolescent Mental Health services and adolescent psychiatrist Dr. Lynette Hsu, the IOP will offer a higher level of care, suitable as a middle ground treatment for patients transitioning to different levels of care. Patients going from more intense levels of care such as residential treatment or hospitalization will have an easier transition to regular outpatient work. The IOP also helps adolescents whose symptoms have not greatly improved from weekly outpatient care. “Patients may be having difficulty getting better or having their symptoms significantly reduced with just regular outpatient care, so the IOP is great if they need a step up [in the] level of care,” Hsu said.
The IOP will accommodate up to eight teens at a time and be offered on a rolling basis. According to Hsu, this intimate, small-group setting effectively fosters stronger relationships between patients and their mental health providers. The program will run for 12 weeks, four times a week from 3 to 6:15 p.m., enabling teens to keep their daily routines as normal as possible.
While it is not mandatory for patients to disclose their participation in the program with their respective schools, the strenuous time commitment may result in scheduling conflicts. However, mental health providers are sworn to confidentiality by law and will only share information with the permission of the patients. This is where communication plays a key role in the success of overall improvement, according to Hsu. “We would encourage communication with schools because people get better when they receive support from more than one area in their life,” she said. “School is such a big part in a teenager’s life and it’s a lot of time to be in a program, so the school could make accommodations to make it more accessible for teenagers to be in such an intensive program.”
Another unique feature to CHC’s IOP is its basis on Dialectal Behavior Therapy (DBT), a therapy designed to be particularly effective among individuals struggling with behaviors that interfere with their normal activities and life pursuits. Unlike other forms of therapy, DBT is very support-oriented, placing a heavy emphasis on collaboration and learning how to regulate emotions. Its multiple components incorporate individual, group and multi-family therapy. “There is a feel-safe learning component, which is typically taught in a group, an individual therapy component and a parent-skill component,” Hsu said. “Because we’re talking about teenagers, parents and family are very important.”
CHC psychologist Dr. Anna Parnes described how a typical day in the program starts off with a check-in and snacks. “The first part of the day is more experiential and about practicing mindfulness by doing mindfulness movement and mindfulness art,” she said. Considering that patients are coming directly from school, expressive forms of art such as dance and poetry give patients the opportunity to stay grounded. The latter part of the day transitions to a skills training group where patients learn coping and problem solving skills.
The components are all led by licensed clinicians and therapists who specialize in working with teens. In addition to group therapy and phone coaching, weekly individual therapy and medication management run by psychiatrists like Dr. Hsu are also available to patients. Although patients may often have a history of clinical depression, self-harm or suicidal thoughts, a pre-existing diagnosis is not necessary in order to be admitted into the program. Admittance is based on referrals, be it through self-referral or from a pediatrician or current therapeutic treatment team. According to Dr. Hsu, CHC uses patient referrals and a conversation between the IOP mental health providers and the family to evaluate the patient’s needs. “We encourage people to call the general CHC number and then one of the providers in the program would schedule time to talk in order to understand if our program would be a good fit for their needs,” she said.
According to Dr. Parnes, the IOP will be accepting private insurance. “We’ll be taking insurance and we also have a sliding fee scale because we don’t want cost to be a barrier,” she said.
While the IOP is a significant milestone in filling a crucial gap in the high demand for local mental health services, CHC strives to continue expanding its services.